7 Foods That Cause Inflammation
7 Foods That Cause Inflammation
HEALTH
MrTruth.Tv
9/18/20257 min read
Inflammation is part of our body’s defensive toolkit — tackling infections, healing wounds, and protecting tissues. But when inflammation persists, it becomes a silent driver for many chronic diseases: cardiovascular disease, type 2 diabetes, some cancers, autoimmune conditions, and more. Diet plays a central role in tipping this balance either toward chronic inflammation or toward wellness.
Recently, new studies have sharpened our understanding of which foods or dietary patterns most contribute to inflammation — and conversely, which foods help calm it. Below, I look at seven categories of foods linked in recent research to elevated inflammation, include expert commentary, and provide novel findings.
Additionally, I describe ideas for infographics that could accompany this article to help readers visualize the risks and trade-offs.
Seven Foods (or Food Types) That Promote Inflammation
The categories below are drawn from recent peer-reviewed studies, cohort data, randomized interventions, and expert consensus. Each section includes mechanisms, evidence, and where possible quotes or findings.
Sugar & Sugar-Sweetened Beverages (SSBs)
What counts: Sodas, sweetened fruit drinks, energy drinks, sugary desserts, high-fructose corn syrup, added refined sugars.
Mechanism:
Sharp glucose spikes → high insulin → oxidative stress.
Formation of advanced glycation end products (AGEs) which can activate inflammatory pathways.
Alteration of gut microbiome, endotoxin exposure.
Recent Evidence:
A large U.S. study (NHANES-based) found that diets higher in sugar and refined carbs showed elevated C-reactive protein (CRP), independent of obesity status. (Referenced in Diet Review: Anti-Inflammatory Diet, Harvard T.H. Chan School of Public Health) The Nutrition Source+1
In a study on the prevalence of pro-inflammatory diets among Americans, Rachel Meadows (Ohio State University) reported that “Even if you’re eating enough fruits or vegetables, if you’re having too much alcohol or red meat, then your overall diet can still be pro-inflammatory.” Sugar-sweetened beverages were among the food items pushing many Americans into pro-inflammatory diet scores. College of Public Health
Typical Impact: Regular consumption of SSBs increases risk of insulin resistance, higher inflammatory markers (CRP, IL-6), weight gain, fatty liver disease.
Refined Carbohydrates & High Glycemic Foods
What counts: White bread, white rice, many breakfast cereals, pastries, refined flour products, sugary baked goods.
Mechanism:
Low fiber → fast absorption → blood sugar spikes.
High glycemic load contributes to insulin sensitivity deterioration and oxidative stress.
Adversely affects gut bacteria that rely on fiber; lower short-chain fatty acid production.
Recent Evidence:
From Diet Review: Anti-Inflammatory Diet (Harvard), refined carbohydrates are explicitly named among foods to limit to reduce inflammatory response. Even after adjusting for obesity and total calories, refined carbs remain associated with higher inflammation markers. The Nutrition Source+1
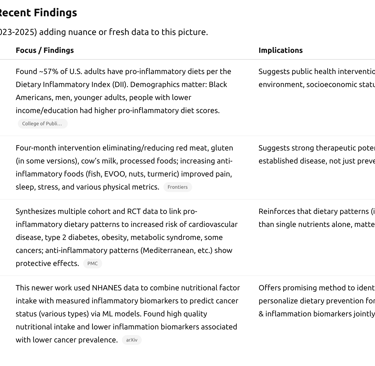
A study of chronic pain patients (AnMeD-S intervention) found that reduced intake of refined grains was one of the beneficial changes correlating with lower pain and improved quality of life. Frontiers
Red Meat & Processed Meats
What counts: Beef, pork, lamb; processed versions like sausages, bacon, hot dogs, deli/cured meats.
Mechanism:
High saturated fat content → promotes pro-inflammatory cytokine production, especially in adipose tissue.
Processing (smoking, curing) introduces nitrates/nitrites, potential carcinogens, oxidized lipids.
Cooking at high heat yields more AGEs and heterocyclic amines.
Recent Evidence:
The Overview of anti-inflammatory diets and their promising effects on noncommunicable disease (2024) outlines that red and processed meats are consistently implicated in studies associating “pro-inflammatory dietary pattern” with heightened risk of cardiovascular disease and type 2 diabetes. PMC+1
In the AnMeD-S pilot study among rheumatic disease patients, eliminating or drastically reducing red meat correlated with improvements in sleep quality, pain, and other metrics. Frontiers
Trans Fats & Excess Saturated Fats
What counts: Partially hydrogenated oils (though many countries limit these now), fried snacks, certain baked goods; excess saturated fat from fatty meats, high-fat dairy, butter.
Mechanism:
Trans fats have well-documented roles raising LDL, lowering HDL, enhancing inflammatory gene expression.
Saturated fat, especially in visceral fat, may interact with Toll-like receptor pathways (e.g., TLR-4), triggering immune cells.
The omega-6 to omega-3 ratio becomes unbalanced, which may promote pro-inflammatory eicosanoid synthesis.
Recent Evidence:
The Harvard diet review lists margarine, shortening, lard (sources of saturated/trans fat) among foods to limit. The Nutrition Source+1
The AnMeD-S intervention also involved reductions in saturated fats, with observed associations with reduced weight, waist circumference, body fat, etc. Frontiers
Ultra-Processed Foods
What counts: Foods high in artificial additives, preservatives, flavorings, colorings; ready-to-heat or eat snacks; processed cereals; many frozen meals; fast food; highly refined packaged products.
Mechanism:
Multiple hits: high sugar, unhealthy fats, salt, additives.
Possible effects on gut barrier integrity.
Likely promotion of dysbiosis in microbiome.
High caloric density → weight gain → adipose tissue inflammation.
Recent Evidence:
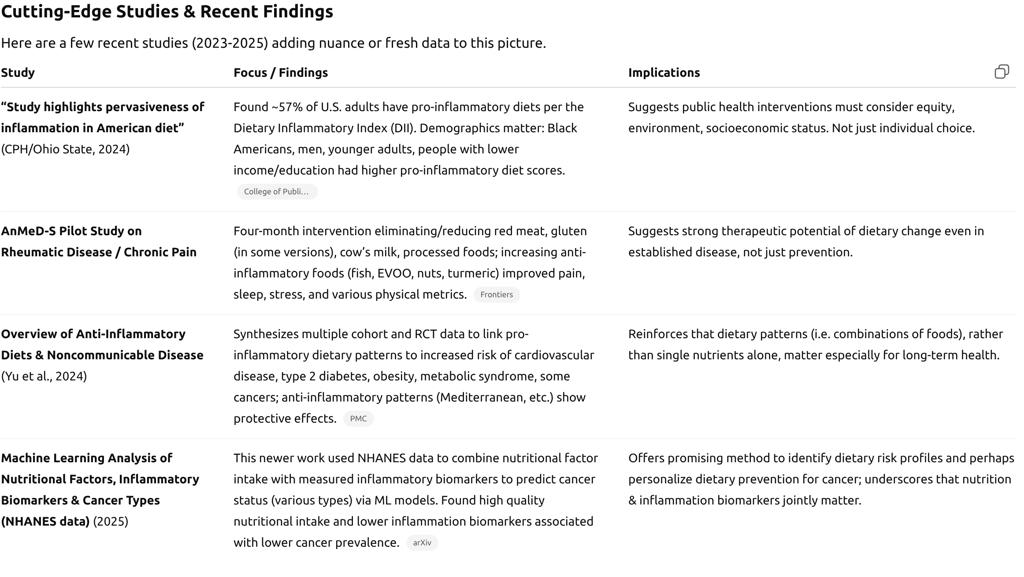
The 2024 study from Ohio State about pro-inflammatory diets reported that ~57% of U.S. adults follow distinctly pro-inflammatory diets, largely characterized by high ultra-processed food consumption. College of Public Health
In AnMeD-S, participants were asked to reduce processed foods; this was among the pro-inflammatory foods whose lower consumption showed association with improved anthropometric and quality-of-life measures. Frontiers
Fried Foods / Foods Cooked at High Temperatures
What counts: Deep-fried items (French fries, fried chicken, etc.), charred meats or fish, grilling to high “blackened” levels, some high-heat sautéing in poor quality oils.
Mechanism:
High temperature cooking creates AGEs, heterocyclic amines, oxidized lipids which are pro-oxidant and can trigger inflammation.
Frying in reused oil or at excessively high heat increases the level of oxidized fats.
Recent Evidence:
Harvard’s review again includes “French fries and other fried foods” among foods to avoid. Harvard Health+1
In cohort data analyzed in Overview of anti-inflammatory diets associations are stronger in people consuming more fried foods, independent of other risk factors. PMC
High Omega-6 / Low Omega-3 Ratio & Certain Vegetable Oils
What counts: Corn oil, soybean oil, sunflower oil (especially when used in processed/packaged goods), diets that include far more omega-6 than omega-3 fatty acids; also the products that use these oils under high heat.
Mechanism:
Omega-6 fatty acids (like linoleic acid) can be converted into pro-inflammatory eicosanoids; when omega-3s (EPA, DHA, ALA) are low, the balance shifts.
Some oils when oxidized contribute to lipid peroxidation and oxidative stress.
Recent Evidence:
From the Overview of anti-inflammatory diets (2024), balancing polyunsaturated fats is discussed: diets high in omega-3s reduce inflammatory markers, while those overly reliant on omega-6 without counterbalance tend toward higher inflammation. PMC
The AnMeD-S study included increased consumption of blue fish and high-quality oils (e.g., extra virgin olive oil) and saw improvements in inflammatory symptoms. Frontiers
Quotes & Expert Commentary
Putting a face on the data, here are some insights from researchers and nutrition experts:
Rachel Meadows, Visiting Faculty, Ohio State University:
“Overall, 57% of U.S. adults have a pro-inflammatory diet … Even if you’re eating enough fruits or vegetables, if you’re having too much alcohol or red meat, then your overall diet can still be pro-inflammatory.” College of Public Health
Dr. Frank Hu, Professor of Nutrition and Epidemiology, Harvard T.H. Chan School of Public Health:
“Some of the foods that have been associated with an increased risk for chronic diseases such as type 2 diabetes and heart disease are also associated with excess inflammation.” Harvard Health
“It’s not surprising, since inflammation is an important underlying mechanism for the development of these diseases.” Harvard HealthFrom the AnMeD-S study authors: In describing improvements seen in patients with chronic pain when pro-inflammatory foods are reduced and anti-inflammatory foods increased, one line reads:
“Better health prognosis … was associated with improved physical variables for cardiometabolic risk … withdrawals of pro-inflammatory foods was significantly associated with … decrease in weight, BMI …” Frontiers
Infographic Ideas
To help readers visually digest the findings, here are some suggested graphics / infographics you could pair with the article:
“Inflammation Trigger Wheel”
A circular diagram with 7 wedges, each representing one of the food categories (e.g. sugar, red meat, fried foods, etc.), showing the mechanisms (insulin spike, AGEs, saturated fats, etc.) and consequences (higher CRP, etc.).“Before & After: AnMeD-S Pilot Study Outcomes”
Bar graphs or a set of small panels showing improvements in pain, sleep, stress, BMI, weight, etc., comparing baseline vs 4 months.“Dietary Inflammatory Index (DII) Heatmap”
Show which demographic groups (age, income, education, race/ethnicity) tend to have more pro-inflammatory diets, from the Ohio State study.“Top 7 Foods to Limit vs 7 Foods to Favor”
Split-screen infographic: left side lists the 7 food types that increase inflammation; right side shows their anti-inflammatory counterparts (e.g. for red meat → fatty fish & legumes; for refined carbs → whole grains; for fried foods → steamed/baked etc.).“Omega-6 vs Omega-3 Balance”
A bar or ratio graphic showing typical Western diet ratio vs recommended balanced ratio; examples of dietary sources.
Updated & More Nuanced Takeaways
Given these new findings, there are some refined observations:
It’s not just "bad" foods, but combinations & context. Even people consuming some healthy foods (fruits/vegetables) can still be in a pro-inflammatory state if they offset with high amounts of sugar, processed foods, or red meat. As Meadows said.
Short-term dietary changes can have measurable effects: As shown in the AnMeD-S trial, in just four months, reductions in pro-inflammatory foods + increases in anti-inflammatory ones led to improvements in pain, sleep, stress.
Socioeconomic and demographic disparities are real: The Ohio State study highlights that lower-income, lower-education, younger, and certain racial/ethnic groups are more likely to have diets high in inflammation. Access, cost, food environment, culture all matter.
New tools and metrics help personalize risk: Research using ML on large data sets (like the NHANES cancer-nutrition-inflammation study) suggests we may be moving toward personalized dietary risk profiling based on both what people eat and their measured inflammatory biomarkers.
Taste, convenience, cost & culture remain barriers: Many people find it easier to reduce something being bad (pro-inflammatory foods) than to completely adopt all recommended anti-inflammatory foods. Education, policy, food environment changes are needed.
What to Do (Practical Advice, Updated)
Putting all this together, here are refined practical steps:
Prioritize reducing the worst offenders first: sugar-sweetened beverages, ultra-processed foods, fried foods, processed meats. These often deliver the most bang per “bad bite” in terms of inflammation.
Replace rather than simply remove:
Swap refined grains with whole-grain options.
Swap red/processed meats with fish, legumes, poultry.
Use cooking methods that avoid high heat damage.
Include foods with known anti-inflammatory effects:
Fatty fish (salmon, sardines, mackerel)
Extra virgin olive oil, nuts, seeds
Berries, leafy greens, colorful vegetables
Spices such as turmeric, ginger, garlic
Monitor portion sizes and overall pattern: Even healthy foods, in excess, may contribute to caloric overload.
Measure what you can: If possible, follow biomarkers (blood sugar, CRP if available, etc.), perhaps under medical supervision, to see if dietary changes are working.
Address systemic and environmental barriers: Cost, food deserts, cultural preferences – these may require policy, community interventions (e.g., accessible fresh produce, education).
Summary
The last few years have reinforced what many nutritionists have argued for decades: chronic low-grade inflammation is intricately tied to what we eat — not just in isolated foods, but in our overall eating patterns. The seven categories listed — sugars, refined carbohydrates, red & processed meats, trans/saturated fats, ultra-processed foods, fried/high-heat cooked foods, and high omega-6 / low omega-3 ratios — consistently show up in studies as drivers of inflammation.
But the good news is: change is possible. Clinical trials (e.g., AnMeD-S), large cohort studies, and new data tools (DII, ML applied to NHANES) demonstrate measurable benefits even over a matter of months. And while individual choice is crucial, the broader food environment, policy, socioeconomics, and culture play big roles. Tackling inflammation through diet is both a personal health strategy and a public health priority.


